There’s no denying that as we grow older our aging hormones can take their toll on our physical health and appearance, both inside and out. While we tend to think of aging as the physical attributes of wrinkles, sagging skin, thinning hair and just overall general malaise, there are internal changes that take place as well that can often times present themselves in other ways.
Because of this, when we think of aging, we have to consider the role that our hormones play when it comes to our health and wellbeing and understand that the symptoms among men and women will vary in a multitude of ways.
The Relationship Between Hormones and Aging
The aging experience, while with some similarities, can be entirely different for men and women. While sleep changes may be consistent for both, for women there’s the well-known stage of menopause, while men experience a less heard of stage of andropause. While both natural occurrences, these two experiences have one commonality; diminished hormone levels.
Hormones That Fluctuate with Age
The endocrine system is composed of multiple organs and tissues that produce hormones throughout the body, and are released into the body to aid in organ or system function. These hormone-producing glands are found in the brain, as the pineal gland, pituitary gland, and hypothalamus, and in the neck, with the thyroid and parathyroid glands. Other key parts of this system include the thymus, the adrenals, the pancreas, and the testes/ovaries. All of these parts produce specific hormones, which function as chemical messengers.
As the body ages, both men and women experience natural changes within the body’s systems that affect the amount or ability that specific hormones are produced, which ultimately affect who the body functions and how well systems perform. These are some of the hormones that are affected for both men and women as they age.
 Produced and released into the bloodstream via the pituitary gland in the brain, TSH controls production of the thyroid hormones, thyroxine and triiodothyronine. Although thyroid levels and TSH, in particular, can change over the course of a year with the seasonal changes, intriguingly, as men and women age, thyroid function decreases as these TSH levels increase with age, even in those without thyroid disease such as hypothyroidism.
Produced and released into the bloodstream via the pituitary gland in the brain, TSH controls production of the thyroid hormones, thyroxine and triiodothyronine. Although thyroid levels and TSH, in particular, can change over the course of a year with the seasonal changes, intriguingly, as men and women age, thyroid function decreases as these TSH levels increase with age, even in those without thyroid disease such as hypothyroidism.
With an increase in age, marked changes in thyroid hormone production, metabolism, and action occur. Thus, resulting in an increased prevalence of (subclinical) thyroid disease in the elderly.
Produced in the four tiny glands located around the thyroid, PTH affects calcium and phosphate levels, which affect bone strength. Like TSH levels, parathyroid hormone levels rise with age, and as a result, may contribute to increased risk of osteoporosis as you age.
The rate of HGH, or GH, secretion from the anterior pituitary gland in the brain is at its highest levels of production around the time of puberty, and thus as we get older, these GH levels decline gradually each year. Decreased levels of this hormone may, most noticeably, lead to decreased muscle mass and strength, and an increase in body fat, thus the continued popularity of increasing HGH levels through dietary changes, supplements and hormone injections.
Melatonin levels decline gradually over the life-span of men and women and may lead to lowered sleep efficacy, and disrupted sleep-wake cycles, also known as circadian rhythms. Unlike many other aging hormone declines which require hormone replacement therapy (HRT) to overcome however, melatonin declines can be compensated for with quality melatonin supplements, ideally in the formulation of a pulsatile-release as to mimic the body’s natural production supply.
A hormone that helps regulate fluid and electrolyte balance, aldosterone release declines with advanced age. This hormonal decrease can contribute to lightheadedness and drops-in blood pressure.
Cortisol is the “stress response” hormone. It affects the breakdown of glucose, protein, and fat, and it has anti-inflammatory and anti-allergy effects. Cortisol release also decreases with aging, but the blood level of this hormone stays about the same. While cortisol fluctuations can be a struggle to manage, there are natural approaches to manage these levels to maintain proper body functions such as proper sleep, balanced nutrition, frequent exercise and decreasing stress.
Like so many other hormones in the body, DHEA levels also tend to decline as men and women age. This drop in DHEA hormone levels has been implicated in age-associated cognitive decline, advanced aging and internal hormone imbalances.
Produced in the small intestine in response to the presence of fat and protein, this hormone is responsible for suppressing the appetite and over time, secretion of and responsiveness to this hormone increases. The role of increased plasma CCK concentrations in mediating a decrease in appetite as we age is still being researched to ascertain correlation, but it is associated with aging as this fluctuation may contribute to the slowing of gastric emptying, mediated by increased pyloric motility.
Produced in the stomach as a response to fasting, this hormone’s function aids in increasing appetite and plays an important role in regulating the energy homeostasis. Opposite to CCK, Ghrelin levels slightly decrease with age, which can account for a decrease in appetite as we age.
Changes in production and responsiveness of the renin-angiotensin system (RAS) are common occurrences with aging in men and women. These types of RAS changes are decreases in production that predispose elderly individuals to various fluid and electrolyte imbalances as well as acute and chronic kidney injury and disease.
Aging Hormone Fluctuations Specific to Men
Frequently, when we talk about aging hormones, we tend to only consider the traditional notion of the word menopause as a stage in women’s lives, however, both men and women can experience dramatic hormonal changes as they age. Also called “male menopause,” andropause is a condition that occurs when a man’s reproductive organs begin a hormonal production decline. However, andropause isn’t the only role that aging plays on men’s hormones and a number of these biological chemicals can be affected over time.
As men grow older, testosterone levels will naturally go down, in fact, by the age of 30, men’s testosterone levels usually start to go down by one percent every year. A gradual decline of testosterone is typically normal for all men, however an unusually low level of testosterone could mean that andropause is in play, and noticeable symptoms can include erectile dysfunction, decreased sex drive, depression and fatigue, mood swings, increased body fat and reduced muscle mass.
While men’s testosterone levels decline with age, estrogen levels tend to rise, a process is known as aromatase which normally occurs in the fat cells. One of the most noticeable signs that indicate the estrogen levels in a man have gone up include gynecomastia, a condition that can lead to developed breast tissue in men, much as it does for females. For men with a higher body mass index, an extra accumulation of fat is common, specifically around the midsection. In addition, the sexual inability and low sexual desire while also being unable to maintain an erection are also signs of increased estrogen levels.
According to research, though men only have small amounts of this hormone in their system anyway, over time, men’s prolactin levels tend to decrease significantly, creating common impairments in men’s sexual functions. Men who had higher body mass indexes and higher glucose levels tended to have lower levels of prolactin, and this hormones’ fluctuations and concentration levels correlate with BMI, as well as gender.
Aging Hormone Fluctuations Specific to Women
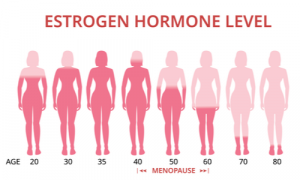
This female reproductive hormone is a key component to women’s cycles, conception, and pregnancy. While progesterone levels fluctuate throughout a women’s cycle, the general levels of this hormone begin declining in women’s late 20s, and decrease significantly after age 30. Similar to estrogen levels, by the stage of menopause, as the ovaries stop hormone production, progesterone levels become nearly nonexistent with advanced age.
Like other reproductive hormones in women, hormone levels fluctuate over time due to the decrease in women’s reproduction phase. Unlike the decline in other hormones however, over time FSH levels actually increase in an attempt to stimulate the ovaries into producing more estrogen. Research has found that the combined raise in FSH and decrease in estrogen levels are the cause for the characteristic hot flashes women experience during menopause.
Like FSH, LH levels rise with age, beginning their increase at about the age of 35 years and maintain at this higher rate until the age of 40 years. The LH levels then increase further in women older than 40 years.
Produced in the pituitary gland, this hormone plays a significant role in lactation as well as other wide-ranging functions in the body, from acting on the reproductive system to influencing behavior and regulating the immune system. With concentration levels depending on BMI, and gender, in women, prolactin levels can remain at a decreased level following menopause.
Healthy Approaches to Hormonal Changes and Imbalances
While hormones tend to have a regular pattern, they follow as we age, there is no singular approach to hormone fluctuations. While some men and women experience textbook hormone declines or increases, there are instances when men and women may have too much or too little of a hormone or a varied fluctuation from the norm. Fortunately, with proper treatment, each symptom, side effect and hormone can help be kept in check and in balance.
To treat hormonal imbalances successfully, general doctors may need to carry out a number of tests to determine whether the imbalance is due to menopause/andropause or another underlying condition. After a successful diagnosis, doctors can look into the most suitable treatment options, or look at specialist referrals if necessary. Aging hormones can cause a number of system fluctuations, and side effect, or stages such as menopause and andropause, and when needed, doctors can work to ensure the best approach for treatment options to manage side effects. In some instances, bioidentical therapy or making necessary lifestyle changes can help keep aging hormones in check.





