New evidence shows that the mitochondria, which provide energy to our cells, also control a DNA repair protein’s ability to suppress the senescence-associated secretory phenotype (SASP), which causes zombie-like cells to secrete pro-inflammatory molecules that can contribute to chronic inflammation in the body. In humans and other multicellular organisms, cells multiply. This crucial feature allows embryos to grow into adulthood and enables the healing of the many bumps, bruises, and scrapes along the way.
How to Prevent Chronic Inflammation Caused by Zombie-Like Cells That Accumulate With Age
Certain factors can cause cells to give up this property and enter a zombie-like state known as senescence. In this state, cells persist but no longer divide to create new cells. Our bodies are adept at clearing these senescent cells, which accumulate as we age. However, the older we get, the less efficient our immune systems are at doing so.
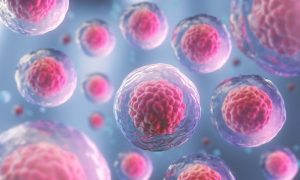
“Besides not growing and proliferating, the other hallmark of senescent cells is that they have this inflammatory program that causes them to secrete inflammatory molecules,” said Peter Adams, PhD, director and professor in the Cancer Genome and Epigenetics Program at Sanford Burnham Prebys and senior and co-corresponding author of the study. Cells “executing” this inflammatory program exhibit the senescence-associated secretory phenotype (SASP). Too many cells with SASP, secreting inflammatory molecules, can contribute to chronic inflammation in the body. This pervasive inflammation – also called “inflammaging” – is associated with many age-related diseases. Sanford Burnham Prebys scientists and colleagues from around the country published research showing that the mitochondria, which supply our cells with energy, also control the ability of a DNA repair protein to suppress SASP, which can reduce or delay inflammatory aging.
Promoting a Healthier Aging Process
The research team exposed human cells to senescence by irradiation and then used these cells to show that the DNA repair protein p53 suppresses SASP and one of its triggering events, the formation of cytoplasmic chromatin fragments (CCF). These fragments are pieces of damaged DNA that have been spewed out of cell nuclei into the gel-like cytoplasm, which occupies the space in the cell between the outer membrane and the central nucleus. The presence of DNA in a place where it doesn’t belong can trigger the immune system and contributes to SASP.
The scientists confirmed their findings in mice by treating them with a drug developed by cancer researchers to activate p53 and thus suppress tumors. In older mice, the drug did not reduce the number of senescent cells, but instead reversed the cellular signature that characterizes age-related SASP, potentially halting the inflammatory burden that can lead to inflammatory aging.
In addition, the researchers found that senescent cells suffer from a dysfunction of mitochondria, which serve as the primary energy source for cells. Stressed mitochondria can cause senescent cells to produce CCF and dampen the expression of the gene that carries the blueprint for p53. Together, we have identified a cellular circuit that is able to promote DNA repair and genome integrity while simultaneously repressing the dangerous inflammatory hallmarks of senescent cells that contribute to age-related disease,” said Karl Miller, Ph.D., a research associate in the Adams laboratory at Sanford Burnham Prebys and senior and co-corresponding author of the study. The researchers also showed that this pathway can be modified by existing drugs in cultured cells and mice, suggesting that it may one day be possible to develop a treatment that targets p53 to promote healthier aging.