Alzheimer’s disease disproportionately affects women, who comprise about two-thirds of those diagnosed with the late-onset form of the disease. Previous research has shown that Alzheimer’s disease is also more severe and progresses faster in women, and that women with Alzheimer’s experience more cognitive decline – loss of memory, attention, and the ability to communicate and make decisions – than men with the disease. The biological basis for these differences between men and women with Alzheimer’s disease has not been well studied. However, understanding them is necessary to develop appropriate therapies.
What Role do Sex Hormones Play in Alzheimer’s Disease?
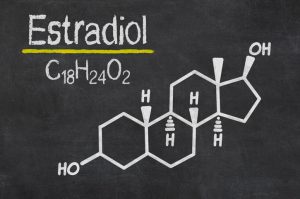
In a study of mice and humans, researchers at Western University have shown that female sex hormones play a significant role in how Alzheimer’s disease manifests in the brain. The study, published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, also highlights the importance of developing therapeutic strategies that focus on these hormonal relationships. The research suggests that the role of estradiol – a form of the female sex hormone oestrogen used therapeutically to relieve menopausal symptoms – in Alzheimer’s disease needs to be better understood.
While the significance of the findings is of utmost importance, the methodology behind it is equally crucial and points to a necessary change in scientific approaches. “To understand the role of sex hormones in Alzheimer’s, we need to study appropriate animal models. Unfortunately, most studies at this level still focus primarily on the male brain. Our research emphasizes the importance of using animal models that reflect postmenopausal females, for example, to understand how sex hormones influence Alzheimer’s pathology,” said Vania Prado, a professor in the Departments of Physiology and Pharmacology and Anatomy and Cell Biology at the Schulich School of Medicine & Dentistry and a scientist at the Robarts Research Institute.
Alzheimer’s and the Brain’s Communication System
One of the key markers of Alzheimer’s disease is the toxic buildup of the protein beta-amyloid in the brain, which eventually disrupts the brain’s communication system and impairs cognition. The new study shows that the brain chemistry of male and female mice regulates the beta-amyloid protein in Alzheimer’s disease in different ways, with the hormone estradiol contributing to this variation. Previous studies in mice and older at-risk individuals have shown that cholinergic neurons, a type of brain cell that produces the chemical messenger acetylcholine, are especially vulnerable to the harmful Alzheimer’s-associated beta-amyloid buildup in the brain. Furthermore, acetylcholine has been shown to be essential for normal memory and cognition.
As beta-amyloid aggregation affects the production of acetylcholine, the subsequent loss of this chemical messenger further intensifies Alzheimer’s pathology, creating a vicious cycle. The Western research team examined this interaction between changes in brain chemistry and the accumulation of beta-amyloid protein observed in Alzheimer’s-affected brains. “Because there are differences in the cholinergic system between male and female brains, we wanted to find out if sex influences this relationship between acetylcholine signaling and beta-amyloid protein buildup,” said Marco Prado, a professor in the Faculties of Physiology and Pharmacology and of Anatomy and Cell Biology. Marco Prado, one of the study authors, is also the Canada Research Chair in Neurochemistry of Dementia and a scientist at the Robarts Research Institute.
Women and Men Respond Differently to Medications and Experience Alzheimer’s Disease in Different Ways
In this study, the researchers observed differences in beta-amyloid accumulation in male and female mice when they altered levels of cholinergic activity. In addition, they analyzed MRI images of the brains of healthy older people. Unlike most studies in humans, in which MRI scans of men and women are analyzed together, Professor Taylor Schmitz and PhD student Hayley Shanks analyzed MRI brain scans and the rate of brain shrinkage in older men and women independently. They observed that the relationship between the integrity of the brain region where cholinergic neurons are located and beta-amyloid accumulation was the same in men and women, but different in male and female mice. The researchers suspected that the fact that the female mice studied were not in postmenopause, while the women were in postmenopause, could be a factor explaining the difference.
The lead author of the study, German-Castelan, was intrigued by the gender differences and decided to introduce another level of testing into the mouse models. With the help of Western researcher Robert Gros, he examined female mice that closely resembled postmenopausal women. This was done to examine how the presence or absence of sex hormones might affect the relationship between cholinergic signaling and beta-amyloid deposition in the brain. The researchers found that when the sex hormone estradiol was present, the relationship between acetylcholine and toxic amyloid was lost, but when the sex hormones were switched off in female mice, this relationship reproduced the results seen in humans.
These results also point to the urgent need to study amyloid and cholinergic function in the “perimenopausal” age group of 40 to 50 years, which is much younger than the individuals studied in most large-scale studies on Alzheimer’s disease. In fact, the average age of the sample studied in this study was closer to 70 years. The researchers emphasized that without including female mice in the study, they might have missed crucial information about Alzheimer’s and gender differences. Women and men respond differently to medications and experience Alzheimer’s disease in different ways. According to the researchers, in order to develop more effective therapies, animal models must be studied that can reproduce various aspects of the disease. Sex hormones and estradiol levels are just one of these factors.