Researchers at the University of Wisconsin-Madison have developed a promising technique for treating osteoarthritis that involves therapeutic blood clots activated by messenger RNA.
New Treatment Technique for Osteoarthritis
Osteoarthritis is a degenerative joint disease caused by the breakdown of cartilage. It affects approximately 600 million people worldwide, making it a leading cause of disability. Osteoarthritis is the most common form of arthritis. It occurs when the cartilage in key joints such as the knee and hip deteriorates, causing pain and stiffness and limiting mobility. The exact mechanism of cartilage breakdown in osteoarthritis is not known, but it is thought that damage from mechanical stress with insufficient self-repair is the main cause. In an article in the journal Bioactive Materials, the UW-Madison research team, led by William Murphy, professor of biomedical engineering and orthopedics and rehabilitation, describes their new approach.
If developed further, it could one day provide a more effective option than treatments such as steroid or hyaluronic acid injections or even joint replacement surgery. In the best case, according to Murphy, this could be an injectable or implantable treatment for patients with advanced osteoarthritis, which would be an alternative to existing treatments that generally do not have high long-term success rates.
Clinical Trials in Humans Planned
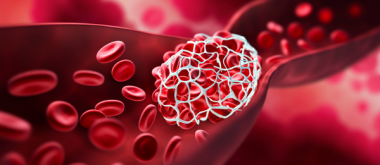
Drawing on his lab’s previous work on mRNA-based vaccines, spinal cord injury therapies and more, the method relies on mineral-coated microparticles that deliver mRNA, which codes for the production of a protein that supports cartilage formation. First, the team takes bone marrow aspirate (liquid bone marrow) and peripheral blood samples from a patient, mixes in the microparticles, and then forms the mixture into a blood clot. The mRNA-activated clot is then placed at the site of the damage. This is all done during the same surgery, and materials derived from the patient are used.
While existing treatments such as arthroscopic chondroplasty can lead to the formation of new fibrocartilage tissue, this material does not have the same mechanical properties as articular cartilage. It also degrades more quickly. However, in contrast to conventional approaches to tissue engineering, the new method does not require a synthetic scaffold material on which cells can grow. After the successes in rabbit models, the group will test their treatment strategy in a larger animal model before proceeding to clinical trials in humans. Murphy says that his group is also investigating the same approach for the treatment of large skeletal muscle and bone defects.