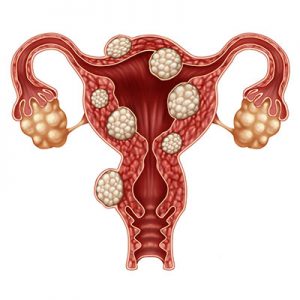
Uterine fibroids are non-cancerous myomas, or growths, that attach themselves to the inside of the uterine wall. These benign growths can cause a woman to have lower abdominal swelling and pressure, prolonged periods of bleeding during menstruation, pelvic and/or lower back pain, pain during intercourse and increased urination. These growths can be as small as a pea and virtually unnoticeable or a large mass that distends the uterus.
Why do Fibroids Develop?
Hormones Play a Key Role
The two hormones implicated in triggering fibroid growth are estrogen and progesterone. Although they are the force behind fibroid growth, these hormones are necessary for developing into a woman and reproduction.
- Estrogen: Responsible for the development of female sexual characteristics and the same hormone that triggers the egg release each month from the ovaries.
- Progesterone: The other major female hormone produced by the ovaries aids in thickening and preparing the uterine lining for the fertilized egg by secreting particular proteins during the second half of the menstrual cycle.
Perimenopause Versus Menopause
The time in a woman’s life when the ovaries stop producing eggs and the production of female hormones of estrogen and progesterone begins to decline marks a time of physical change. Women can reach this stage of reproductive cessation as early as in their 40s and even into their 60s with an average age of complete termination of about 51 years old.

Once reaching the menopausal state as levels of estrogen and progesterone decline, uterine fibroids and the discomfort associated with them may lessen. Although the growths will still remain present in the uterus, the size will often dissipate and new fibroid growth may be stunted. With that being said, there are some risk factors that can increase fibroid development after the end of menstrual cycles. They include:
- High blood pressure
- Low vitamin D levels
- Family history
- Obesity
- No history of pregnancy
- Excessive stress
- Hormone replacement therapy
Fibroid Treatment
Treatment for fibroids can vary from pain management with non-steroidal anti-inflammatory medications to introducing birth control pills in premenopausal women. However, once postmenopausal, introducing any type of hormone therapy can have an adverse effect on fibroid growth. Procedures such as myomectomy (removal of myoma) or embolization (cutting off blood supply to the fibroids) have been found to benefit some women. In severe cases, doctors may even recommend a hysterectomy, i.e. removal of the uterus and/or ovaries.
With many variants of risk factors and severity of fibroids, the best course of action is to consult your physician and discuss the pros and cons of the treatment that is best for you.





